Addiction Treatment for Heroin and Opioid Painkillers
Facing treatment for heroin addiction can be scary, and the thought of facing reality without the crutch of drug addiction that the addict has come to rely on can be paralyzing. It is far easier to stay caught up in the madness of chasing more heroin than it is to stop using heroin entirely and learn a new way to live. While recovery from heroin addiction may feel difficult to begin and, later, exceptionally challenging to maintain, selection of the right treatment options can greatly facilitate the process. Recovery from heroin is indeed possible, and a number of treatment options are available to help if you want it.
What Are Opioid Drugs?
The opioids are in a class of drugs that act to give the body relief from pain, but also may cause the user to experience a pleasurable sense of euphoria in the brain. Heroin is one commonly abused illicit opioid. Other abused opioids include the prescription painkiller drugs – administered by doctors for managing a number of painful health conditions.
Those who abuse heroin and those who abuse prescription painkillers are alike in that both have developed dependency on an opioid drug.
Some of these prescription opioid drugs include:
- Oxycodone (OxyContin, Percocet).
- Hydrocodone (Lortab, Norco, Vicodin).
- Morphine (Avinza, Kadian).
- Codeine (Tylenol 3).
Some individuals begin using these medications as prescribed for pain. But then eventually, these individuals begin to abuse their access to these drugs and eventually develop a substance dependency. In this way, those who abuse heroin and those who abuse prescription opioid drugs are alike – both have developed dependency on an opioid drug.
What Is Opioid Dependence?
Dependence is not exactly the same thing as addiction. Physical dependence develops because the body has developed a normal adaptation to chronic drug exposure.
Dependence can develop with many drugs, including painkiller prescription drugs – either when abused or when taken as prescribed. Drug addiction indeed includes physical dependence. But it also includes compulsive drug-seeking behaviors and drug use, even in the face of devastating consequences.
In the case of either isolated physical dependence or full-blown addiction, unpleasant withdrawal symptoms are likely to occur when drug use is suddenly reduced or stopped.1 Research shows that long-term drug abuse results in changes in the brain that persist long after a person has stopped using drugs.2 These drug-induced changes to the brain are an indication of opioid dependence.
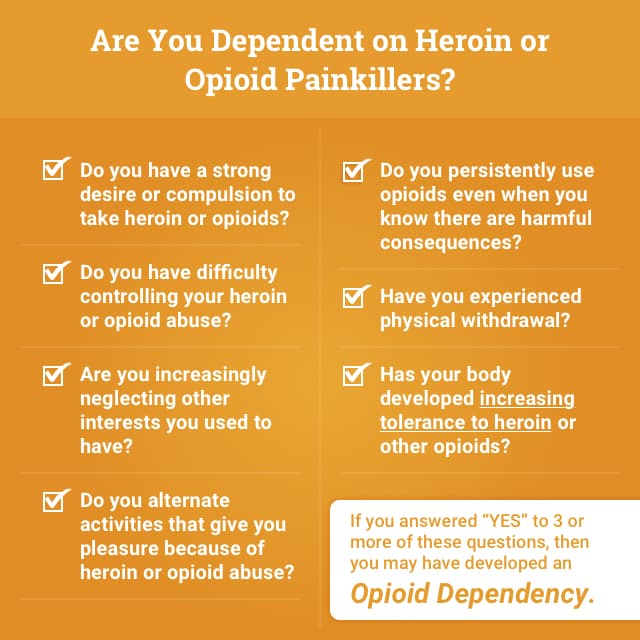
Opioid dependence is characterized by the presence of 3 or more of these symptoms or behaviors:
- A strong desire or compulsion to take opioids.
- Difficulties controlling opioid use.
- Increasing neglect of other interests.
- Persistent use of opioids even when it is clear that there are harmful consequences.
- Tolerance to the opioid used.
- Experiencing physical withdrawal.3
What Is the Goal of Treatment?
Effective treatment programs typically incorporate many components.
Comprehensive addiction treatment must help an individual to stop using drugs, to maintain a drug-free lifestyle and to re-establish productive functioning in the family, at work and in society.2
Research has shown that individuals successfully become engaged in treatment through phases of outreach, initiation into a treatment program, engagement in the treatment process, pharmaceutical/behavioral therapy and aftercare.
Goals of treatment typically include the following:
- To reduce or stop drug use.
- To improve physical and emotional health.
- To make meaningful contributions to the community through employment.
- To improve social functioning and relationships.4

There is no one best treatment for everyone. The best treatment program will be individualized to address your particular set of needs in addition to addressing the underlying drug abuse.5
Why Is Treatment Needed to Get off Opioid Dependence?
The main reason for undergoing a medically-assisted or supervised treatment – instead of attempting to tackle your opioid dependence alone – is that treatment professionals can more adequately monitor your body’s detox process and help to reduce your opioid withdrawal symptoms. Common opioid withdrawal symptoms include:
- Drug cravings.
- Moodiness: anxiety, depression, fear of withdrawal.
- Stomach cramps.
- Upper body secretions: runny nose, watery eyes, perspiration.
- Restlessness: yawning, insomnia.
- Diarrhea.
- Fever and chills.
- Muscle spasms, joint pain, tremor.
- Nausea and vomiting.
- Cardiovascular problems: increased heart rate and blood pressure.
Addiction has an underlying biological cause, which explains why it can be very difficult to achieve and maintain abstinence without treatment. Intense cravings for drugs can be triggered by stress from work or relationships or from environmental cues such as smells, objects or scenes from past drug abuse. Any of these triggers can reduce the ability to successfully maintain abstinence, making relapse more likely. Active participation in treatment is important for successful outcomes, and even the most severely addicted individuals can succeed if they are fully engaged.3
What Does the Treatment Process Usually Look Like?
The best treatment plan will depend on an individual’s particular needs as well as the types of drugs that have been taken.
Treatment can take different forms; it can also take place in a variety of settings and can last for differing periods of time.3 For many, treatment takes place over a period of time, involving multiple interventions and regular monitoring.
Treatments over longer durations have been shown to be associated with improved outcomes for recovering individuals.4
Research has suggested that staying in treatment for less than 90 days is less effective than treatment of longer durations.
Throughout treatment, an individual’s progress must be continually assessed so treatment adjustments can be made in response to evolving needs.5
Where Does Treatment Occur?
Recovery from opioid dependence can be accomplished in any of the following settings:
- Inpatient hospital setting: for intensive, around-the-clock, overnight medical care.
- Outpatient services: for participating in a treatment plan while living at home.
- Residential facilities: for temporary housing provision where you can receive attentive care and therapy alongside a focused and supportive recovery environment.
The decision of where to undergo treatment should be determined, in part, by each individual’s unique set of problems and level of needs.6
Withdrawal and Detox
During the detoxification stage, the body attempts to rid itself of any residual drug in the body. This phase can be quite challenging physically and psychologically, especially when attempted alone.
Since the body is suddenly deprived of the drug it’s grown used to relying on, it goes through a series of uncomfortable withdrawal symptoms as it readjusts to a new “normal” without the drug.
Though determined by the specific drug that is abused, withdrawal symptoms can be expected to appear 6-12 hours after one’s last opioid use. Pharmaceutically tapered detox can last anywhere from 4 hours to 4 weeks.
What Drugs Are Used During Withdrawal and Treatment?
Medication is an important part of treatment and can be combined with counseling or other behavioral treatment for even greater effectiveness.
Medication can serve different purposes at different stages of treatment – for stopping drug abuse, for staying in treatment or for avoiding relapse.
Medication-assisted treatments (MAT) can include opioid agonists, opioid antagonists and alpha-2 agonists. These drugs have been shown to be effective medications for opioid addiction treatment – whether one’s addiction is to heroin or to opioid prescription painkillers.7 Some medications appear to be more effective and safe than others.
Let’s verify your coverage for treatment at an American Addiction Centers location. Your information is always confidential.
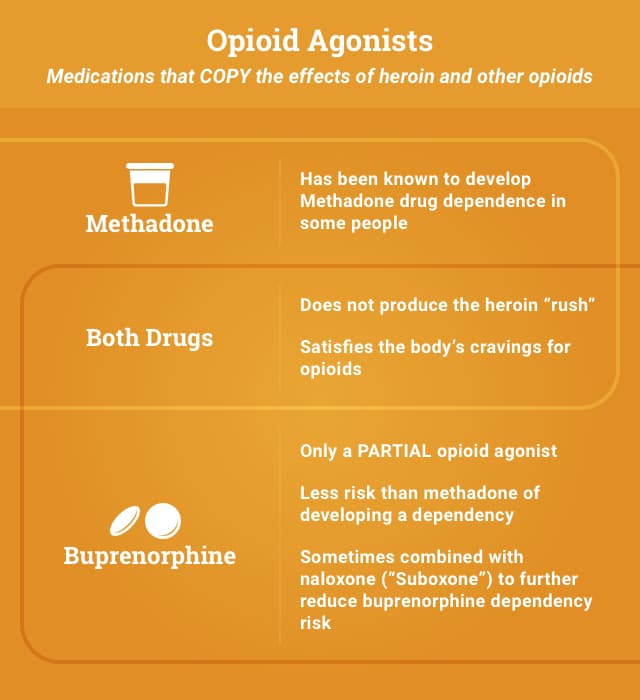
Opioid Agonists
Opioid agonists are medications that copy the effects of heroin and other opioids. Methadone is a full opioid agonist, and buprenorphine is a partial opioid agonist. Both are used in treatment for addiction to heroin and other opioids.
Methadone
Methadone is a long-acting opioid agonist medication. As an addiction treatment pharmaceutical, methadone is taken orally. The drug activates the same receptors as heroin and other opioids. By activating the same receptors, it ends up mimicking some of the effects of heroin. Since methadone works slower and with less intensity than heroin, however, it does not give heroin’s same “rush” sensation but still satisfies the body’s cravings for opioids.
Buprenorphine
Buprenorphine is a partial opioid agonist medication that works similarly to methadone, in that it does not produce a “high” but still relieves opioid cravings. Buprenorphine is able to reduce or eliminate withdrawal symptoms associated with opioid dependence and, with only partial agonist activity, carries a low risk of overdose.
Physicians who have a Drug Enforcement Administration (DEA) waiver to provide this type of care can administer buprenorphine as a treatment in office-based settings.
When combined with naloxone – an opioid antagonist (or blocker) – the risks of overdose or abuse are further minimized. A combined formulation of buprenorphine and naloxone is marketed under the trade Suboxone.
Suboxone is believed to more greatly reduce possible risks of overdose or abuse, compared with buprenorphine alone.
Implantable Buprenorphine?
According to USA Today, in January 2016, a new implantable form of buprenorphine (“Probuphine”) was proposed to the U.S. Food and Drug Administration. One problem with the existing pill or dissolvable film form of the drug has been that those receiving these drug forms have been known to sell these supplies in exchange for other drugs.

Braeburn Pharmaceuticals, the manufacturer of “Probuphine,” argues that the implant would reduce that risk. Similar to contraceptive implants, the implant provides a steady dose of the drug over a period of 6 months after insertion.
Only one clinical study has been done so far on the drug that reported an even higher effectiveness rate than the dissolvable film – however, some have claimed that the study was poorly done and has some missing data.
Time will tell if implantable buprenorphine becomes a commonplace opiate treatment of the future.
Other Medications
Naltrexone(opioid antagonist)
Naltrexone is a non-addictive opioid antagonist, meaning that it works by blocking the effects on heroin and other opioids. It’s been used for many years to reverse opioid overdose and is approved for use in the treatment of opioid addiction.
Treatment for reducing withdrawal symptoms usually begins during the detoxification process and may occur in outpatient, inpatient and residential settings.
Experienced clinicians find that naltrexone works best for highly motivated and recently detoxified patients who desire total drug abstinence.
Naltrexone is sometimes prescribed in outpatient settings to be taken three times a day, but sometimes patients have trouble following through visiting the outpatient clinic so frequently. A new, long-acting injectable version of naltrexone – called Vivitrol – has also been approved to treat opioid addiction, however. This version of the drug needs to be delivered just once a month – a frequency that makes follow-through easier for patients. Some have reported, however, that naltrexone may not be as effective as some of the other opioid agonist drugs available for treatment (such as buprenorphine).9
Clonidine(alpha-2 agonist)
Other drugs such as clonidine have offered an alternative medication option for those undergoing opioid withdrawal. Clonidine works very differently than the other medications listed above, as it is an alpha-2 adrenergic receptor agonist and does not work on opioid receptors at all.
Alpha-2 agonists slow the heart rate, lower blood pressure, reduce muscle tone and can cause drowsiness or sedation.10
Clonidine and other alpha-2 agonists (e.g., lofexidine and guanfacine) act on the nervous system by reducing the neurotransmitters adrenaline and noradrenaline – the “fight or flight” chemicals that are present in larger amounts in the body during opioid withdrawal.
Technically, clonidine is not actually FDA-approved for treating opioid withdrawal in the U.S. – but it is often still used for this purpose.
Rapid Opioid Detoxification
Some individuals seek the speediest method of detox available, even though these speedier detox options have been reported as being among the most dangerous detox options.
Rapid opioid detox (ROD) quickly induces withdrawal through monitored administration of opioid antagonists such as naloxone or naltrexone plus clonidine.
Physical discomfort is reduced through the use of sedative hypnotic agents or general anesthetics.
Rapid Opioid Detox: Is It Safe?
It has been observed that rapidly infused naloxone can cause a sudden release of catecholamines in certain individuals – and in some cases, where these “fight or flight” chemicals have been strong enough to cause pulmonary edema or cardiac arrhythmias.11
A 2005 public policy statement from the American Society of Addiction Medicine says that “further research into the physiology and consequences of ROD should be supported so that patients may be directed to the most effective treatment methods and practices.” 12
Anesthesia-assisted Opioid Detoxification
Anesthesia-assisted opioid detoxification, or ultra-rapid opioid detoxification (UROD), is another speedy detox option that uses large doses of naloxone to cause the fastest possible opioid withdrawal in an opioid user.
This process puts individuals under general anesthesia during an intense administration of naloxone.
Physical elimination of the opioid drug can occur in as little as 4 to 8 hours. Patients experience mild withdrawal symptoms for about 6 days after awakening from anesthesia – compared with similar withdrawal symptoms on a 20-day methadone taper.
The Guideline Committee of the most recent guidelines of the American Society of Addition does not recommend UROD due to high risk for adverse events or death.13 In one study, it was shown that among those who underwent anesthesia-assisted rapid detox, 8.6% of these individuals developed either a cardiac arrest or died. 14
In one study, it was shown that among those who underwent anesthesia-assisted rapid detox, 8.6% of these individuals developed either a cardiac arrest or died.
Beyond Withdrawal and Detox
It should be noted that getting through the withdrawal and detox stage alone does not mark the end of the recovery process, as it will not guarantee the important behavioral changes needed to maintain a drug-free lifestyle. While it is an important first step, successful recovery is often best achieved in conjunction with behavioral therapy and additional supports.
Behavioral Therapy
Examples of behavioral therapy are those that try to get patients to recognize, avoid and cope with situations where they are most likely to want to abuse drugs. Sometimes positive reinforcement is given to patients for staying drug free. Motivational interviewing and group therapy may also be additional components of behavioral therapy.
Additional Supports
For recovery to be effective, it should also be accompanied by a supportive environment and supportive counseling. Appropriate symptom management should also be provided to further develop an individualized treatment plan.4 The best programs offer other services beyond those specifically focused on the issue of substance abuse. These additional services may include:
- Medical support.
- Dual diagnosis treatment and care for multiple medical, mental and behavioral health conditions you may be simultaneously facing.
- Individual or group counseling.
- Family therapy.
- Parenting support.
- Recovery support groups.
- Social services.
- Legal services.
- Aftercare that prepares individuals for life after recovery.
Maintenance Treatments
Maintenance treatment is a consistent schedule of pharmacotherapy for people with addiction.
This therapy is often conducted with the use of an opioid agonist or partial agonist (such as methadone or buprenorphine discussed above).
Maintenance treatment serves the purpose of helping an individual to achieve a steady state where addictive substances are no longer sought for reward and/or relief.
Maintenance treatments of addiction are also designed to protect against the risk of overdose. Depending on one’s particular circumstances, a care plan including maintenance treatments may be time-limited, or it may remain in place for life. 13
Learn More and Connect with Help
If you or someone you love has been struggling with addiction to heroin or other opioid drugs, take comfort in the fact that you are not alone in your struggle. There are many treatment and support options available to help you safely and comfortably break free from this dependency. Call to speak with one of our caring recovery advisors who can help answer any questions you might have and help you in your next steps towards recovery.
Sources
- National Institute on Drug Abuse. (2001). Prescription drug abuse. drugabuse.gov (Vol. 33).
- World Health Organization. (2009). Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence.
- National Institute on Drug Abuse. (1999). Principles of Drug Addiction Treatment: A Research-Based Guide. Third Edition.
- Ali, R. (2010). Pharmacological Treatment. In Atlas on Substance Use (2010) Resources for the prevention and treatment of substance abuse disorders (pp. 57–74). World Health Organization.
- National Institute on Drug Abuse. (2009). DrugFacts: Treatment Approaches for Drug Addiction, (September), 1–5.
- National Institute on Drug Abuse. (2011). Seeking Drug Abuse Treatment?: Know What To Ask Seeking Drug Abuse Treatment.
- National Institute on Drug Abuse. (2015). The Prescription Opioid Epidemic and Heroin. Retrieved November 23, 2015.
- National Institue on Drug Abuse. (2012). Opioid Addiction. Retrieved November 23, 2015.
- Schottenfeld RS, Chawarski MC, Mazlan M (2008). Maintenance treatment with buprenorphine and naltrexone for heroin dependence in Malaysia: a randomized, double-blind, placebo-controlled trial. Lancet, 371 (9631). 2190– 2200.
- Gold MS, Pottash AC, Sweeney DR, Kleber HD. Opiate withdrawal using clonidine. A safe, effective, and rapid nonopiate treatment. JAMA. 1980;243(4):343.
- Van Dorp E, Yassen A, Dahan A. Naloxone treatment in opioid addiction: the risks and benefits. Expert Opin Drug Saf. 2007 Mar;6(2):125-32.
- American Society of Addiction Medicine. (2005). Public Policy Statement On Rapid and Ultra Rapid Opioid Detoxification. Retrieved November 25, 2105.
- American Society of Addiction Medicine. (2015). National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use. American Society of Addiction Medicine, 33, 1–64.
- Collins ED, Kleber HD, Whittlington RA, Heitler NE. Anesthesia-assisted vs buprenorphine- or clonidine-assisted heroin detoxification and naltrexone induction: a randomized trial. JAMA 2005;294(8):903.
Heroin Rehabilitation Directory
Select a state to learn more about your treatment options.- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- District Of Columbia
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- West Virginia
- Wisconsin
- Wyoming
Help for Heroin Addiction
Do you know someone suffering from heroin addiction? Help is available. To find out more, please choose the selection that applies to you or the person suffering from addiction:
Fill out the form below to be contacted.
Repair the damage and start fresh today!